When I first started working in revenue cycle management, one of the biggest challenges I noticed was how often claims were delayed or denied because of modifiers. These two-digit codes may seem small, but they carry a lot of weight in how a claim is processed. Over the past five years, I’ve worked closely with practices to improve reimbursements, and one consistent lesson has been this: if modifiers are not used correctly, you will see avoidable denials.
In this blog, I want to share a practical breakdown of the types of modifiers in medical billing, along with examples from real-world scenarios that providers and billing teams deal with every day.
What Exactly Are Modifiers?
Think of a CPT or HCPCS code as the headline of a story. It tells payers what procedure or service was performed. But sometimes the headline isn’t enough. That’s where modifiers step in, they add the important details that explain how, where, or under what circumstances the service was provided.
For example, if a physician performs two procedures during one visit, you can’t just submit the codes as-is. Without the right modifier, payers might bundle them together and pay less than what’s owed. The right modifier makes sure the claim tells the full story.
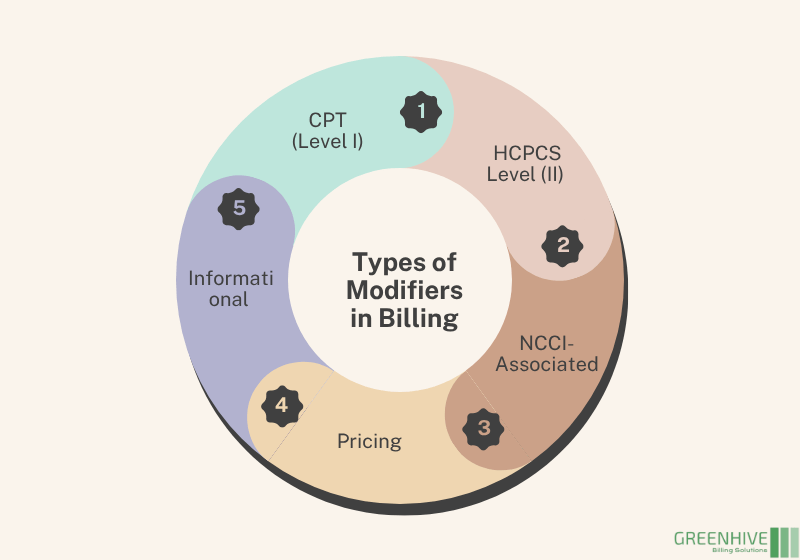
The Main Types of Modifiers You’ll See in Billing
Over the years, I’ve noticed that most coding errors come from not knowing which type of modifier applies. Let’s walk through the main categories:
1. CPT Modifiers (Level I)
These are numeric modifiers created by the AMA. They’re the ones you’ll probably use most often in practice.
- Modifier 25 – A common one in clinics. It shows that an E/M service was provided separately from a procedure on the same day.
- Modifier 51 – Used when multiple procedures are done in the same session.
When I worked with a family practice, we saw denials drop significantly after tightening up the use of Modifier 25.
2. HCPCS Level II Modifiers
These are alphanumeric and often relate to equipment, supplies, or anatomical sites.
- LT (Left Side) and RT (Right Side) – mark which side of the body was treated.
- E1–E4 – specify eyelids (upper left, lower left, etc.).
I’ve seen these especially important in ophthalmology and orthopedics, where side specificity makes all the difference.
3. NCCI-Associated Modifiers
The National Correct Coding Initiative prevents “unbundling” of services. But sometimes procedures that usually bundle together truly are distinct. That’s when modifiers step in.
- Modifier 59 – Distinct Procedural Service.
- Newer subsets like XE, XS, XP, XU are used for even more clarity.
I always remind billing teams: Modifier 59 is one of the most audited, so it should only be used when documentation fully supports it.
4. Pricing Modifiers
These directly affect how much reimbursement you get.
- Modifier 26 – Professional component (e.g., interpreting a test).
- Modifier TC – Technical component (e.g., equipment and staff).
One imaging center I worked with had major payment delays because they weren’t distinguishing between 26 and TC correctly. Fixing that improved cash flow almost immediately.
5. Informational Modifiers
These don’t usually change payment but give payers important context.
- Modifier 24 – Unrelated E/M during a postoperative period.
- Modifier 33 – Preventive services.
Even if they don’t impact pricing, they help avoid extra documentation requests and reduce payer back-and-forth.
The Modifiers I See Most Often
In day-to-day billing, a handful of modifiers appear repeatedly. Here are the ones I usually train teams to pay the most attention to:
- 22 – Increased Procedural Service
- 25 – Separate E/M Service
- 26 / TC – Splitting professional and technical work
- 50 – Bilateral Procedure
- 51 – Multiple Procedures
- 59 – Distinct Procedural Service
Get this right, and you’ll avoid a large percentage of common denials.
Why Modifiers Matter So Much
For me, the importance of modifiers boils down to three things:
- Cleaner claims, fewer denials. Every correctly applied modifier is one less resubmission.
- Proper reimbursement. Providers deserve to be paid for the full scope of services delivered.
- Audit protection. Misused modifiers, especially 25 and 59, can trigger compliance red flags.
I’ve seen practices improve their bottom line significantly just by focusing on proper modifier use. It may feel like a small detail, but it’s one that directly impacts revenue.
My Best Practices for Working with Modifiers
Here’s what I always recommend to the teams I work with:
- Use official references – CPT Appendix A and HCPCS Level II are your guide.
- Stay current – Medicare and commercial payers update modifier rules frequently.
- Back everything with documentation – Never use a modifier without clinical support.
- Provide refresher training – Even experienced coders can fall into bad habits.
- Know payer-specific rules – Not all insurers treat modifiers the same.
My Takeaway from Experience
After working in healthcare billing for years, I can say that understanding modifiers is one of the simplest ways to strengthen a revenue cycle. They may be just two characters long, but they make the difference between an underpaid claim and a fully reimbursed one.
If you’re a provider or billing professional, I encourage you to take a closer look at how your team is using modifiers. In my experience, even a small adjustment here can make a noticeable improvement in cash flow and compliance.