Did you know that up to 80% of medical bills contain errors, causing costly claim denials and significant revenue loss for healthcare organizations? Achieving high medical coding accuracy remains a persistent challenge, impacting both financial performance and operational efficiency.
This article presents seven essential, actionable tips to help healthcare professionals, clinics, and organizations improve medical coding accuracy and reduce claim denials. From ongoing training to leveraging the right technology, these proven strategies can streamline workflows, minimize errors, and maximize reimbursement.
Read on to discover how to optimize your organization’s coding processes and secure a healthier revenue cycle.
The High Cost of Medical Coding Errors
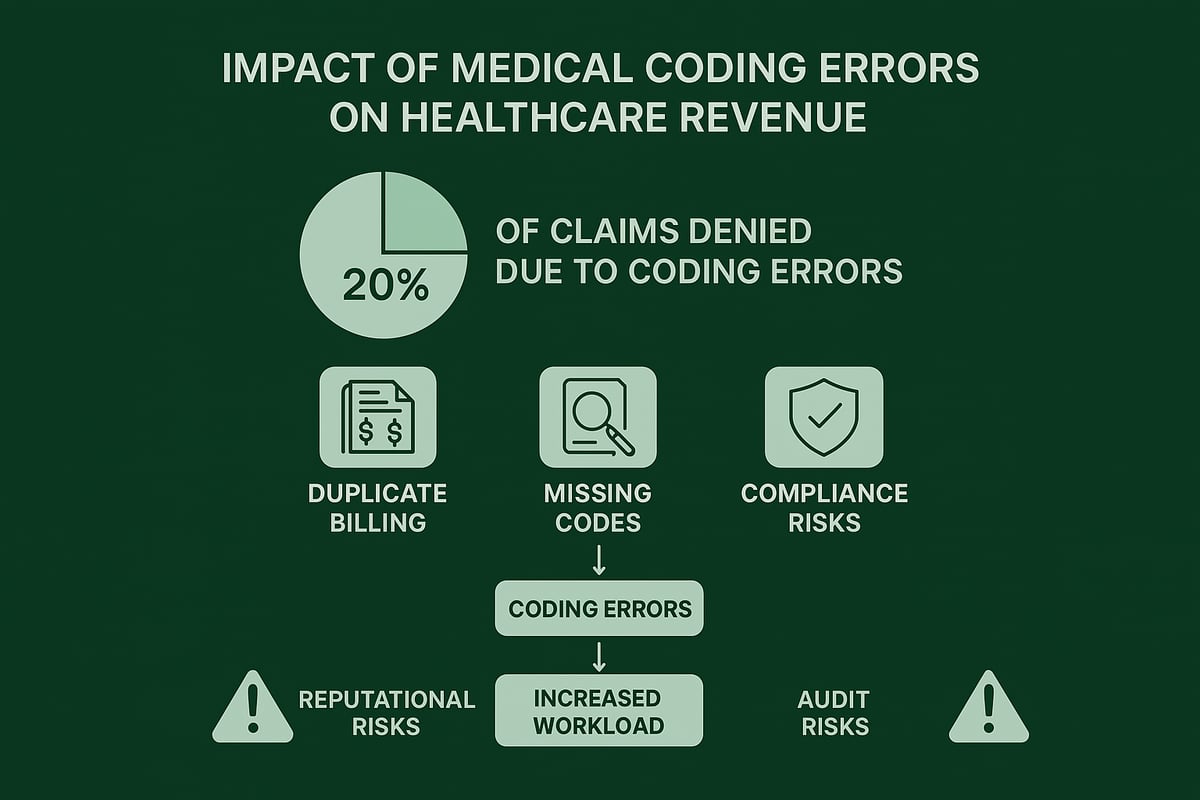
Medical coding accuracy is vital for the financial health of any healthcare organization. Coding errors can have a significant impact on revenue cycle management, leading to costly delays and lost income. Recent industry analysis shows that up to 20% of claims are denied due to coding mistakes, putting millions of dollars at risk each year.
Common errors include duplicate billing, upcoding or downcoding, missing codes, and insufficient documentation. These mistakes not only slow down the reimbursement process but also increase the administrative workload for billing teams. Each denied or delayed claim requires additional resources to resolve, which can strain staff and reduce overall efficiency.
The effects of poor medical coding accuracy extend beyond finances. Frequent errors can damage a practice’s reputation and erode patient trust. Regulatory compliance is also jeopardized when documentation does not meet audit standards or payer requirements.
To understand the full scope of these challenges, review this comprehensive overview of denials in medical coding explained, which highlights the most common causes and their business impact.
With the stakes so high, proactive strategies to improve medical coding accuracy are more crucial than ever for sustainable success.
7 Essential Tips to Boost Medical Coding Accuracy
Enhancing medical coding accuracy is vital for sustainable revenue and operational efficiency. The following seven strategies offer actionable steps for healthcare organizations seeking to minimize claim denials and optimize reimbursement.
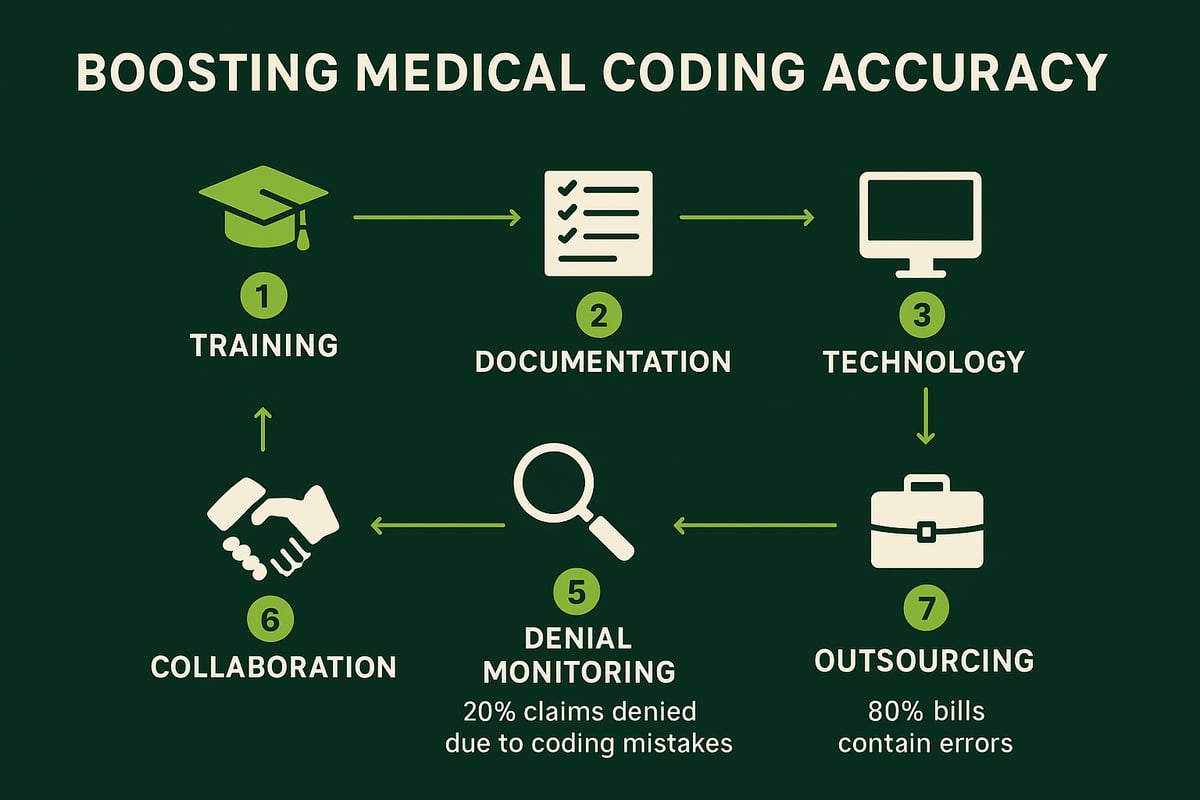
1. Invest in Ongoing Training and Education
Continuous education is the foundation of medical coding accuracy. Regular training ensures that coders and providers stay updated on the latest ICD, CPT, and HCPCS code changes. Addressing payer-specific requirements and annual updates is crucial.
Practices that schedule quarterly training often see a notable drop in denial rates. Encourage your coding team to pursue professional certification and continuing education. Cross-training staff helps maintain workflow when team members are absent.
2. Standardize Documentation Practices
Clear and consistent documentation is essential for accurate code assignment. Implement standardized guidelines for all providers, using checklists and EHR templates to capture every required detail.
Incomplete or vague notes frequently cause claim rejections. Conduct routine audits to spot documentation gaps and provide targeted feedback to providers. Consistency streamlines audits and supports compliance.
3. Leverage Technology and Coding Tools
Utilizing technology is a game changer for medical coding accuracy. EHR-integrated coding tools provide real-time error checking and flag duplicate codes or invalid modifiers.
Automated claim scrubbing software helps reduce errors before submission, minimizing denials. Always keep your technology updated with the latest codes, and ensure integration with your billing and denial management platforms for seamless operations.
4. Conduct Pre-Submission Claim Reviews
Establishing a rigorous pre-submission review process is critical. Use detailed checklists to verify code accuracy, patient and provider information, and modifier use before claims are sent.
Weekly audits can catch frequent errors early, reducing costly rework. Assign experienced staff to oversee final reviews and track recurring issues. Addressing these proactively leads to fewer denials and smoother reimbursement cycles.
5. Monitor Denials and Analyze Trends
Regularly monitoring denied claims is vital for improving medical coding accuracy. Analyze denial data weekly or monthly to identify patterns and recurring mistakes.
Use these insights to inform targeted coder training and workflow adjustments. For example, high denial rates for specific codes or payers signal where corrective action is needed. Sharing findings with the revenue cycle team fosters collective problem-solving and ongoing improvement.
6. Foster Collaboration Between Coders and Providers
Effective communication between coders and providers is central to accurate outcomes. Schedule routine meetings to discuss documentation, coding changes, and payer requirements.
Encourage coders to query providers when clarification is needed, which reduces denials for insufficient documentation. Develop team-based feedback loops to address ongoing challenges and promote a culture of compliance.
7. Consider Expert Outsourcing for Complex Specialties
Some specialties require advanced knowledge and frequent code updates, making outsourcing a smart solution for medical coding accuracy. Bringing in specialized professionals can reduce errors and speed up reimbursement, especially in areas like oncology or orthopedics.
Evaluate the return on investment of outsourcing versus in-house efforts. Ensure your partner is certified, experienced, and HIPAA-compliant. For an overview of how expert outsourcing can elevate your organization’s results, visit our medical coding services overview. Maintain oversight and communicate regularly with your external teams for best outcomes.
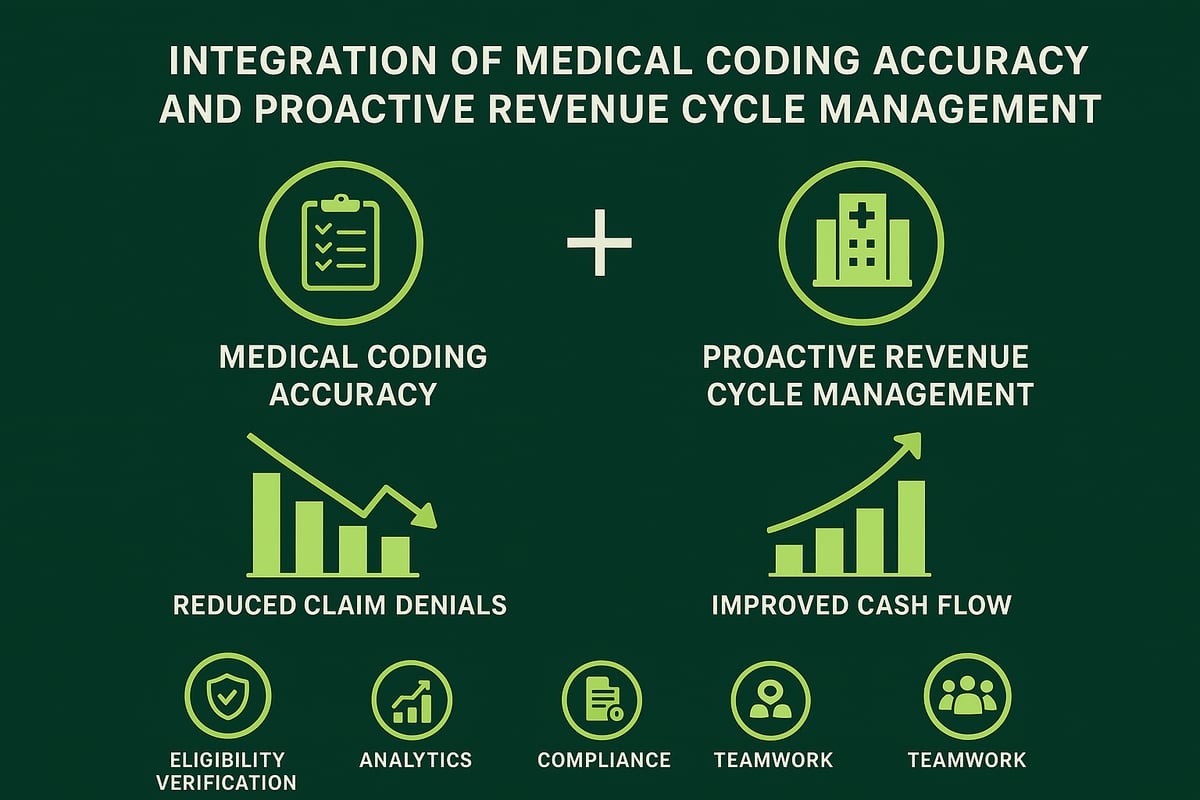
The Role of Proactive Revenue Cycle Management
A proactive revenue cycle management (RCM) approach is essential for maintaining high medical coding accuracy throughout the entire claims process. By integrating coding accuracy into every stage of the revenue cycle, healthcare organizations can prevent errors before they impact reimbursement.
Eligibility verification is the first line of defense. Confirming patient coverage up front helps avoid downstream denials caused by mismatches or outdated information. Real-time analytics and denial management tools are also critical, enabling teams to spot error trends and address issues before they escalate.
Working with an experienced RCM service provider brings additional benefits. Skilled teams can adapt to client-owned software, optimizing existing workflows without requiring a system overhaul. This flexibility ensures that best practices in medical coding accuracy are upheld within each organization's unique environment.
For example, practices that leverage end-to-end RCM support often see fewer claim denials and stronger cash flow. These results come from seamless integration of coding, billing, and denial management—a process explored further in Medical coding and RCM integration.
Regular performance reviews and transparent reporting keep organizations informed and accountable. Staying compliant with HIPAA and evolving payer regulations is a continuous process, not a one-time task.
Ultimately, medical coding accuracy must be viewed as an organization-wide commitment. When every stakeholder—from coders to administrators—prioritizes precision, healthcare practices are better positioned for financial health and regulatory success.
Future-Proofing Medical Coding Accuracy: Trends and Best Practices
Staying ahead in medical coding accuracy means more than following the basics. Healthcare organizations must anticipate industry shifts, regulatory updates, and evolving payer expectations. Proactive strategies help teams adapt, minimize disruption, and consistently meet compliance standards.
Staying Ahead of Regulatory and Industry Changes
The regulatory landscape for medical coding accuracy is always shifting. Annual updates to ICD, CPT, and HCPCS codes, along with payer-specific policy changes, require constant vigilance. Participating in industry forums and subscribing to coding update services keeps your team informed and agile.
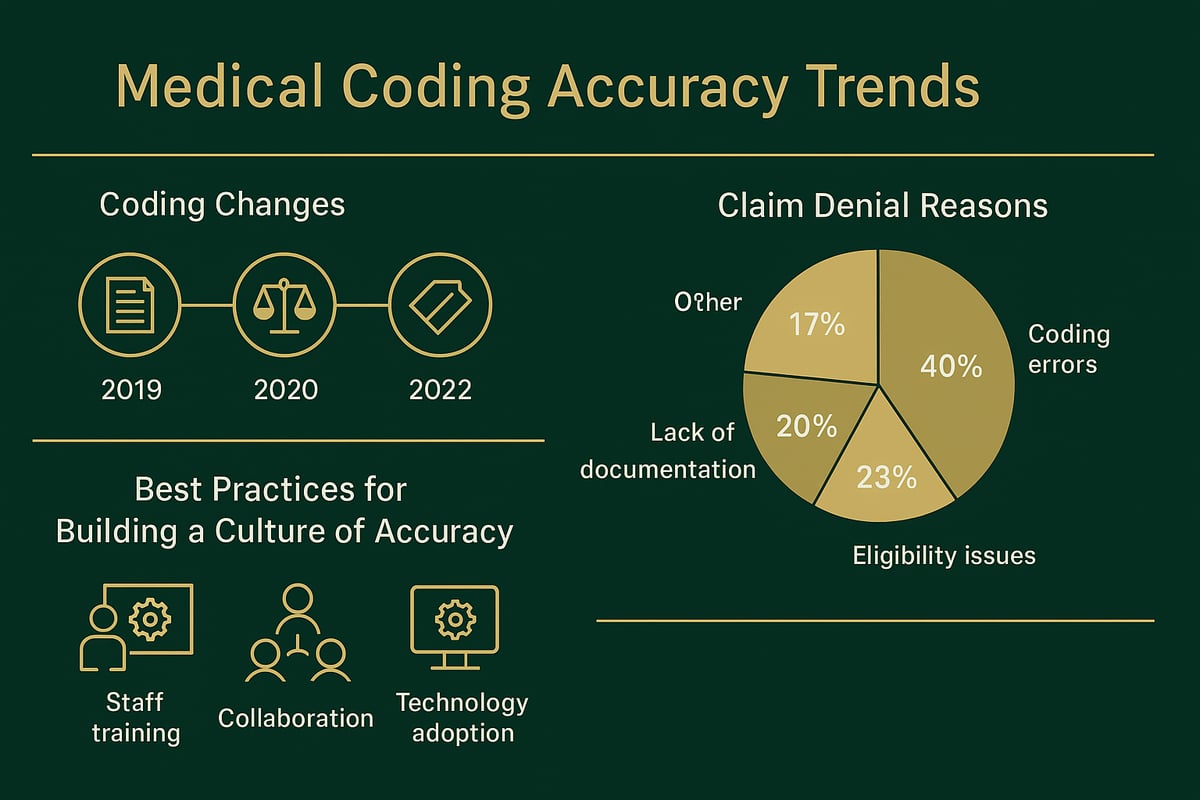
For example, organizations that quickly adapt to new telehealth codes or modifier guidelines avoid unnecessary revenue loss. As highlighted in the MDaudit’s 2024 Benchmark Report, there has been a significant rise in coding-related denials, underscoring the importance of staying current. Continuous process improvement and flexibility help prepare your team for increased scrutiny and more demanding documentation requirements.
- Monitor annual code set and payer policy changes
- Join professional forums, attend webinars
- Regularly review internal workflows for improvement
Adaptation is critical for sustainable medical coding accuracy.
Building a Culture of Accuracy and Accountability
Building a culture centered on medical coding accuracy starts with organization-wide commitment. Recognizing and rewarding coding team achievements fosters motivation and accountability. Ongoing feedback, knowledge sharing, and professional development keep the team engaged and up to date with best practices.
Investing in certification and continuous education demonstrates a dedication to quality and compliance. As detailed in Strategies for Improving Coding Accuracy, regular audits and collaboration are essential for maintaining high standards. When accuracy is valued as a core business asset, healthcare organizations are better prepared for regulatory changes and industry challenges.
- Celebrate coding excellence and milestones
- Encourage open communication across teams
- Support ongoing training and certification
A strong culture of accuracy ensures long-term success in medical coding accuracy.
As you work to improve coding accuracy and protect your practice’s revenue, it’s important to know exactly where your current processes stand. The strategies we covered—from ongoing training to smarter use of technology—are most effective when you understand your unique strengths and challenges. If you’re ready to take the next step toward reducing errors, boosting compliance, and maximizing reimbursements, why not get an objective look at your current workflow? You can start by taking advantage of a Get Your Free Audit with Greenhive Billing Solutions. Let’s make 2026 your most accurate year yet.