When Billing Becomes the Loudest Problem in the Room
Medical Billing Services in Flagstaff, Arizona (AZ)
Reliable Medical Billing Support for Flagstaff Healthcare Providers
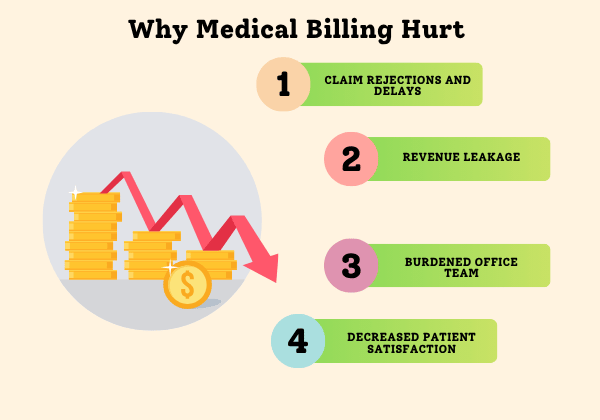
Flagstaff healthcare practices don’t usually notice billing failure all at once. It shows up gradually — slower deposits, unexplained balances, repeated patient questions, and denials that surface weeks after care is delivered. By the time it feels urgent, revenue gaps are already baked into daily operations.
Greenhive Billing Solutions delivers structured medical billing services in Flagstaff, Arizona, designed for practices that need consistency, visibility, and accountability in their revenue process. We don’t rely on assumptions or automated shortcuts, we actively manage claims, payments, and payer communication to prevent revenue from drifting out of reach.
Claims That Go Quiet
Many claims are never formally denied — they simply stop moving. Without structured follow-up, they age past recovery windows.
Insurance Conversations That Lead Nowhere
Staff often hear “processing,” “pending,” or “resubmitted” without real progress. We take ownership of payer dialogue and document every outcome until resolution.
Too Many Hands, No Clear Control
When billing responsibility shifts between people or vendors, work falls through gaps and outcomes become unpredictable.

When Billing Pressure Spills Into Clinical Time
Why Flagstaff Practices Reconsider Their Billing Setup
Outsourcing billing is rarely the first choice. Most Flagstaff practices reach that decision after billing issues begin disrupting patient care and internal trust.
- Front-desk teams stretched between patients and insurance follow-ups
- Providers questioned about denials they didn’t cause
- Owners unsure why revenue reports don’t match visit volume
- Billing issues discovered only after cash flow tightens
Greenhive Billing Solutions assumes full responsibility for billing execution, so your team isn’t forced to absorb payer complexity alongside patient care.
Preventing Revenue Slowdowns Before They Escalate
How Claims and Payments Are Actively Managed
Lost revenue is rarely the result of one large error. It accumulates when claims aren’t revisited, payments aren’t validated, and denials aren’t worked with urgency. Our billing operations are designed to prevent stagnation at every stage.
- Role-based system access to protect workflows and data
- Charge reviews focused on payer-specific acceptance rules
- Ongoing claim follow-up until insurers provide definitive outcomes
- Payment verification against contracted reimbursement rates
- Denials corrected and appealed using repeatable, documented steps
Billing isn’t considered finished when a claim is sent — it’s finished when payment is confirmed and posted accurately.
SERVICES
Small Billing Breakdowns Create Long-Term Revenue Loss
Most revenue shortfalls aren’t dramatic. They come from small breakdowns — secondary claims left unbilled, corrections delayed, or underpayments accepted without review.
Greenhive helps Casa Grande practice
Most practices don’t lose revenue in dramatic ways. They lose it quietly — secondary claims never sent, partial payments accepted without review, or corrections delayed until deadlines pass.
Greenhive helps Flagstaff practices identify where billing momentum slows, intervene early, and restore confidence in revenue reporting.
s pinpoint where billing momentum slows, address issues before they escalate, and rebuild trust in their revenue reporting.
Bringing Stability Back to an Unpredictable Revenue Cycle
How Billing Issues Ripple Across the Practice
Billing problems don’t stay confined to the back office. They affect morale, patient experience, and leadership decision-making.
- Teams experience burnout from recurring billing issues
- Providers lose confidence in billing instructions
- Patients receive confusing or delayed statements
- Leadership struggles to forecast revenue reliably
Stabilizing billing restores predictability and trust across the entire organization.
Replace Guesswork With Repeatable Execution
Building a Billing Operation That Holds Its Ground
Reliable billing isn’t about reacting faster — it’s about working from structured processes that don’t depend on individual memory or constant oversight. Our teams follow defined workflows, stay current with payer changes, and apply Arizona billing standards to keep revenue moving forward without disruption.
BENEFITS
What Practices Notice Once Billing Is No Longer a Daily Distraction
Practices experience measurable improvement without expanding internal staff or increasing leadership oversight.
Problems Surface Sooner
Billing risks are identified before they turn into lost revenue.
Reduced Administrative Drain
Managers no longer need to chase claim status or rework billing tasks.
Faster Reimbursement Turnaround
Claims are actively worked instead of sitting idle.
More Complete Revenue Capture
Missed services and underpayments are consistently recovered.
Keep Billing From Pulling Focus Away From Care
When billing feels unstable, it creates constant interruption. Greenhive manages payer requirements quietly in the background so staff and providers can stay focused on patient care.
Handling Insurance Complexity Without Passing It Back to Your Team
Each payer operates under different rules, timelines, and documentation standards. We manage eligibility checks, authorizations, corrections, resubmissions, and insurer communication — without routing issues back to your staff.
OUTCOMES
Results That Make a Difference
Greater accuracy. Fewer denials. Faster payments.

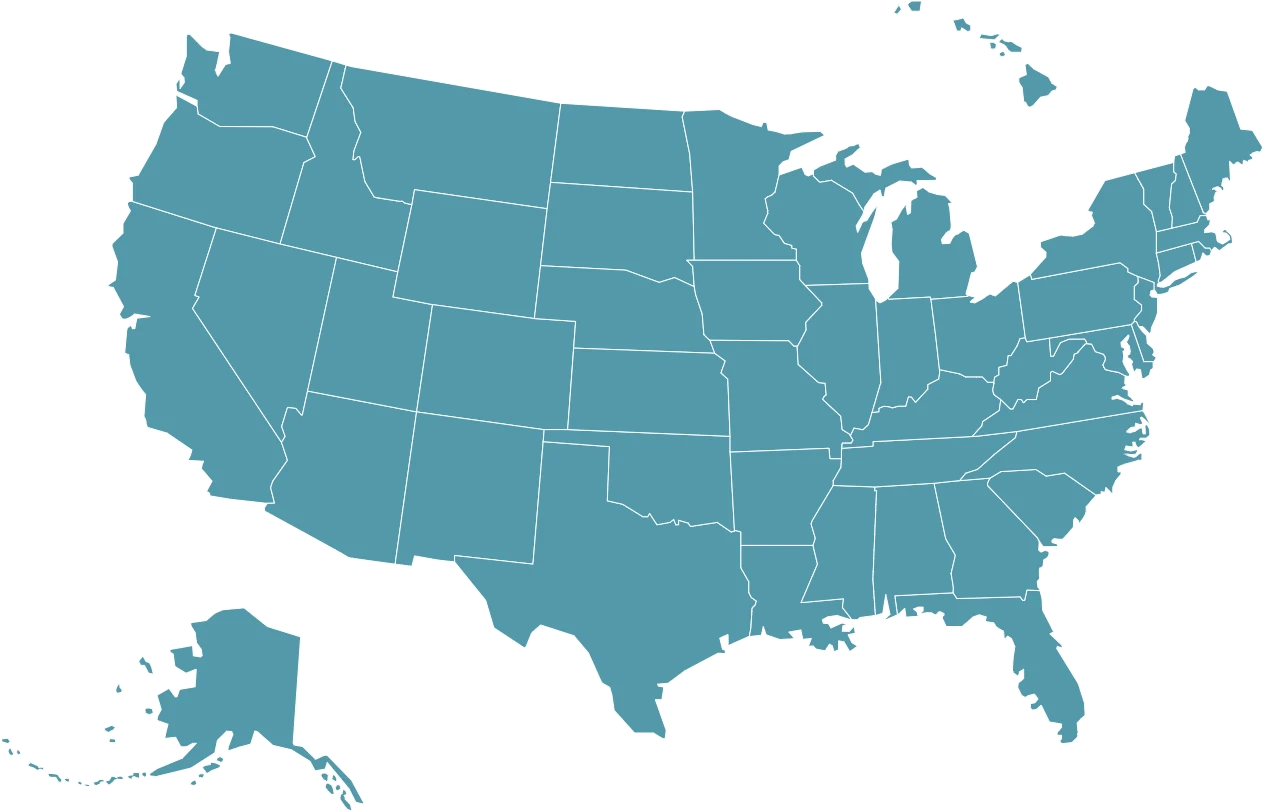
Serving Healthcare Providers Nationwide
Strengthening Revenue Operations Across Practices
Billing instability is one of the most underestimated operational risks in healthcare. Greenhive delivers structured billing execution that keeps revenue moving and issues contained.
ANY QUESTIONS?
Frequently Asked Questions
Does Flagstaff’s payer mix affect billing performance?
Yes. Many practices handle a higher share of Medicare, Medicaid, and regional commercial plans, which requires close attention to authorization rules and documentation timing.
Why do payments sometimes arrive lower than expected?
Underpayments often occur when contracted rates aren’t verified or adjustments go unchallenged. Without review, these losses compound over time.
Can billing results improve without replacing our EHR or PM system?
In most cases, yes. Strong billing performance depends more on workflow discipline and follow-up execution than on the software itself.
WE SUPPORT
From Flagstaff Clinics to Multi-State Operations
Whether you operate a single practice in Flagstaff, AZ or manage providers across multiple locations, Greenhive delivers billing operations built for visibility, accountability, and control.
