Accurate coding for Annual Wellness Visits is more critical than ever in 2026 as policy updates and reimbursement changes reshape healthcare billing. For organizations striving to remain compliant and financially strong, understanding the annual wellness visit cpt code by age is essential.
This article delivers a detailed, age-specific guide to AWV CPT codes for 2026. It is designed to help healthcare professionals, billing teams, and practice managers navigate the latest requirements with confidence.
You will find an overview of CPT codes, age-based breakdowns, key documentation tips, compliance best practices, and the most important updates for 2026. Get ready to strengthen your coding strategy, reduce denials, and improve revenue with this comprehensive resource.
Understanding Annual Wellness Visit (AWV) CPT Codes
Annual Wellness Visits (AWVs) are a cornerstone of preventive care for Medicare and other insured populations. These visits are designed to assess a patient's overall health, identify risk factors, and create a personalized prevention plan. For healthcare organizations, understanding the annual wellness visit cpt code by age is essential to ensure proper billing, compliance, and optimal reimbursement.
What Are AWVs and Why Do They Matter?
AWVs are annual preventive care visits covered by Medicare and many commercial payers. Unlike routine physical exams, AWVs focus on health risk assessment, screening, and long-term wellness planning instead of physical examination or treatment of acute issues. Selecting the correct annual wellness visit cpt code by age ensures that services align with payer requirements and supports preventive care goals.
Key CPT Codes for AWVs
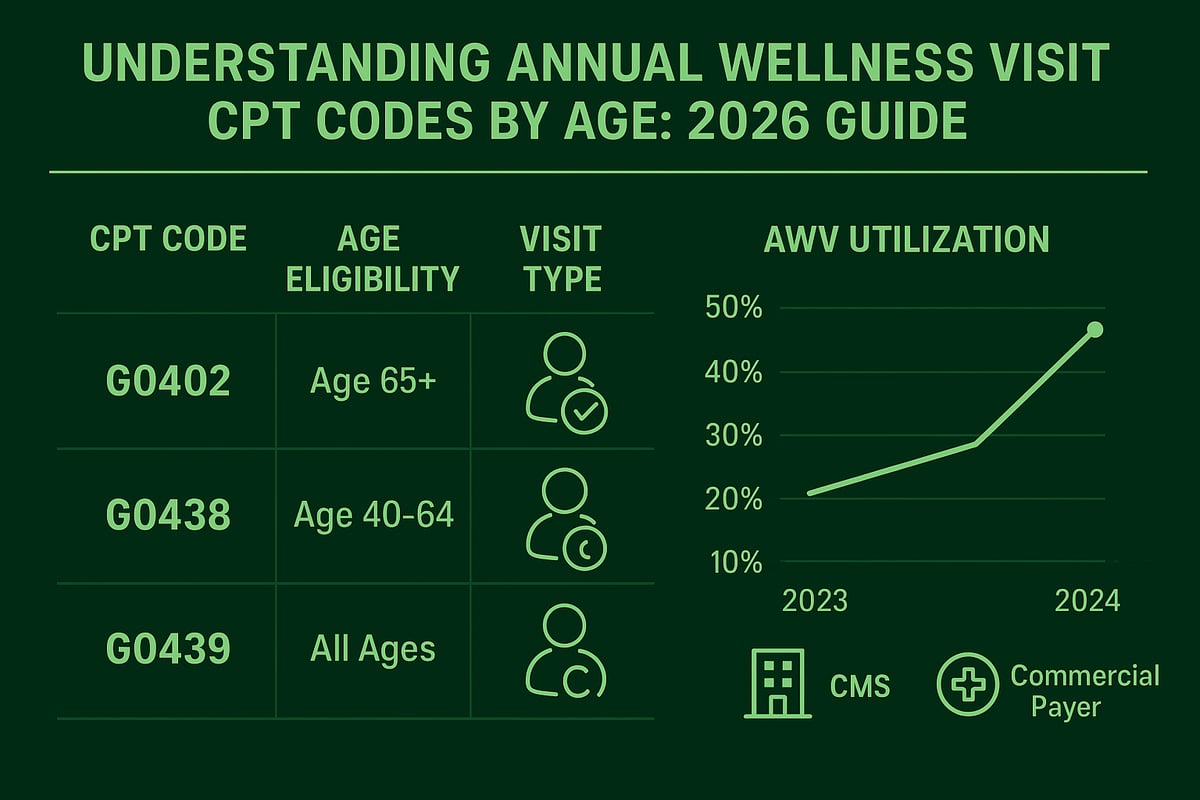
The three primary CPT codes for AWVs are:
| Code | Description | Eligibility |
|---|---|---|
| G0402 | Initial Preventive Physical Examination (IPPE) | New Medicare beneficiaries, first 12 months |
| G0438 | Initial Annual Wellness Visit (AWV) | After IPPE, once in a lifetime |
| G0439 | Subsequent Annual Wellness Visit (AWV) | Annually after G0438 |
Each code has specific documentation and eligibility criteria. For a detailed explanation of how CPT codes function within healthcare billing, see this CPT codes in healthcare claims guide.
AWVs vs. IPPE and Routine Physicals
The IPPE (G0402) is often called the "Welcome to Medicare" visit and is only available within a beneficiary's first 12 months of Medicare Part B coverage. In contrast, the AWV (G0438 for initial, G0439 for subsequent) can be billed annually after the IPPE. Unlike annual wellness visits, routine physical exams are not covered by Medicare and use different codes when billed to commercial payers. Knowing which annual wellness visit cpt code by age applies is crucial for compliant billing.
Medicare vs. Commercial Payer Requirements
Medicare has specific rules for AWV CPT code use based on the patient's age and visit history. Commercial payers may have similar or different policies, sometimes allowing for annual wellness visits at younger ages or covering additional preventive services. Utilization statistics from CMS show that AWV uptake increased by over 15% between 2023 and 2024, reflecting the growing importance of accurate coding.
The Importance of Accurate Code Selection
Choosing the correct annual wellness visit cpt code by age is vital for revenue integrity and compliance. Common errors include:
- Using the wrong code based on patient eligibility or visit type
- Insufficient documentation to support the billed service
- Confusing AWV codes with those for routine physicals
Incorrect coding can lead to claim denials, delayed payments, or audit risk. By understanding the structure of AWV CPT codes and payer requirements, healthcare organizations can minimize errors and ensure optimal reimbursement.
Annual Wellness Visit CPT Codes by Age: A Step-by-Step Guide for 2026
Navigating the annual wellness visit cpt code by age is essential for healthcare organizations seeking accurate billing and optimal reimbursement in 2026. With evolving regulations and payer requirements, understanding how age and visit history impact CPT code selection is critical. This guide walks you through each step, from initial eligibility to nuanced scenarios, to ensure your team codes Annual Wellness Visits (AWVs) confidently and compliantly.
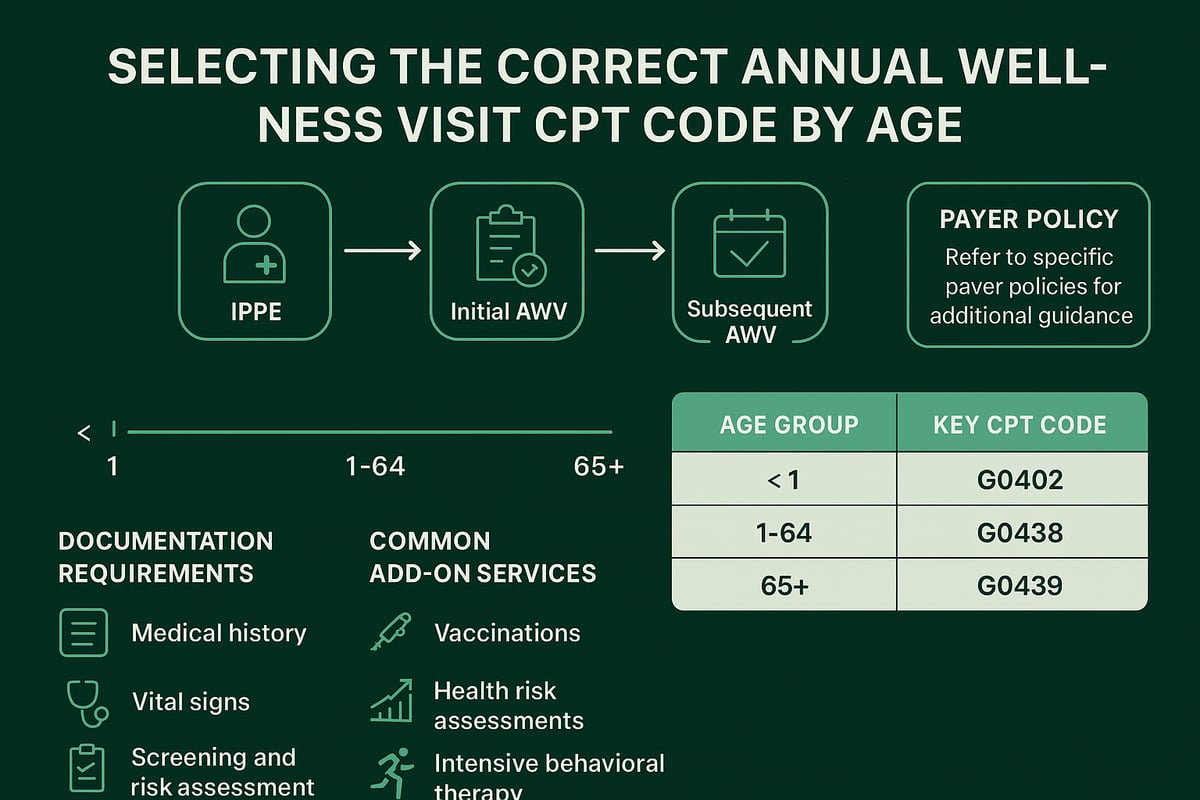
Step 1: Identifying Eligibility for Initial Preventive Physical Examination (IPPE)
The first step in selecting the correct annual wellness visit cpt code by age is confirming if the patient is a new Medicare beneficiary. The IPPE, billed with CPT code G0402, is available once within the first 12 months of Medicare Part B enrollment. This visit is not an annual physical, but rather a one-time preventive service focusing on health risk assessment, medical history, and education on preventive services.
For patients under 65 or those without Medicare, the IPPE does not apply. Ensure your billing team verifies the patient’s Medicare start date and documents eligibility before proceeding.
Step 2: Initial Annual Wellness Visit for Patients New to AWV
After the IPPE window, the next milestone in the annual wellness visit cpt code by age workflow is the Initial Annual Wellness Visit, billed under CPT code G0438. This code is used once in a lifetime for patients who have never received an AWV. It includes a personalized prevention plan, review of medical and family history, and risk factors assessment.
G0438 cannot be billed if an IPPE (G0402) has occurred in the same year. Accurate tracking of prior visits is vital to avoid claim denials and maintain compliance.
Step 3: Subsequent Annual Wellness Visits for Established Patients
For patients who have completed both the IPPE and the initial AWV, annual follow-up visits are coded with G0439. This code is the foundation of the annual wellness visit cpt code by age for established Medicare patients. G0439 covers yearly updates to the prevention plan, reassessment of risk factors, and ongoing screening.
It is essential to confirm that at least 12 months have passed since the previous AWV before billing G0439. Failing to observe this timeline can result in denied claims and lost revenue.
Step 4: Age-Specific Considerations for Pediatric, Adolescent, Adult, and Geriatric Patients
While the annual wellness visit cpt code by age is primarily designed for adult Medicare beneficiaries, it is crucial to recognize payer-specific policies for younger populations. Pediatric and adolescent visits are not covered by AWV CPT codes, but may be billed using codes aligned with Bright Futures guidelines or commercial plan requirements.
For adults under 65 on commercial plans, confirm if the payer recognizes AWV codes or prefers standard preventive visit codes. Geriatric patients (65+) require attention to cognitive assessment and chronic care management, often as add-ons to the AWV.
A helpful reference for these distinctions is the AWV Coding and Billing Guide, which details age and payer-specific coding nuances.
Step 5: Coding Nuances for Dual-Eligible and Commercial Plans
Patients with both Medicare and Medicaid (“dual-eligible”) or those covered by commercial insurance may present unique coding challenges. The annual wellness visit cpt code by age remains the primary guide, but Medicaid or commercial payers may have additional requirements, limitations, or preferred codes.
Always verify the patient’s primary payer, coordinate benefits when necessary, and consult payer-specific bulletins to ensure compliant coding. Some plans may require different documentation or restrict AWV frequency.
Step 6: Billing for Additional Preventive Services During AWV
It is common to provide additional preventive services during an AWV, such as depression screening, cognitive assessment, or advance care planning. While the annual wellness visit cpt code by age determines the main visit code, these extra services are billed separately with their own CPT codes.
Use proper modifiers and document each service distinctly to avoid bundling errors and ensure full reimbursement. Review payer guidelines, as some may require prior authorization or limit same-day billing for certain services.
Step 7: Documentation Requirements for Each Age Group
Accurate documentation supports the annual wellness visit cpt code by age and defends against payer audits. For each visit type and age group, ensure thorough records of health risk assessment, screenings performed, counseling provided, and the creation or update of a personalized prevention plan.
Documentation must align with Medicare, Medicaid, or commercial payer standards. Missing or incomplete records are a leading cause of AWV claim denials, so standardized checklists and regular staff training are best practices.
Table: AWV CPT Codes by Age and Visit Type
| Age Group | Visit Type | CPT Code | Frequency |
|---|---|---|---|
| New Medicare | IPPE | G0402 | Once, within 12 months |
| All Medicare | Initial AWV | G0438 | Once, after IPPE |
| All Medicare | Subsequent AWV | G0439 | Annually, after G0438 |
| Under 21 | Pediatric/Adolescent | Varies | Per payer guidelines |
| Commercial | Preventive Visits | Varies | Per plan policy |
Example Scenarios: Applying the Guide
Consider a 65-year-old new Medicare patient. If within the first year of enrollment, bill G0402 for the IPPE. For a 75-year-old who completed an AWV last year, G0439 is appropriate for the current visit. Dual-eligible patients require careful coordination to determine if Medicare or Medicaid is primary, and which CPT code aligns with the annual wellness visit cpt code by age.
For commercial beneficiaries, consult their plan for the correct preventive visit code, as AWV codes may not apply.
By following this comprehensive step-by-step approach, your organization can maximize compliance, reduce denials, and ensure correct reimbursement for every annual wellness visit cpt code by age scenario.
2026 Updates: Changes and Trends in AWV CPT Coding
Staying ahead of regulatory changes is critical for healthcare organizations, especially with the evolving landscape of AWV CPT coding. In 2026, several important updates will impact how providers approach the annual wellness visit cpt code by age, as well as the compliance and reimbursement process. Understanding these changes is essential for revenue cycle teams, practice managers, and clinical staff.
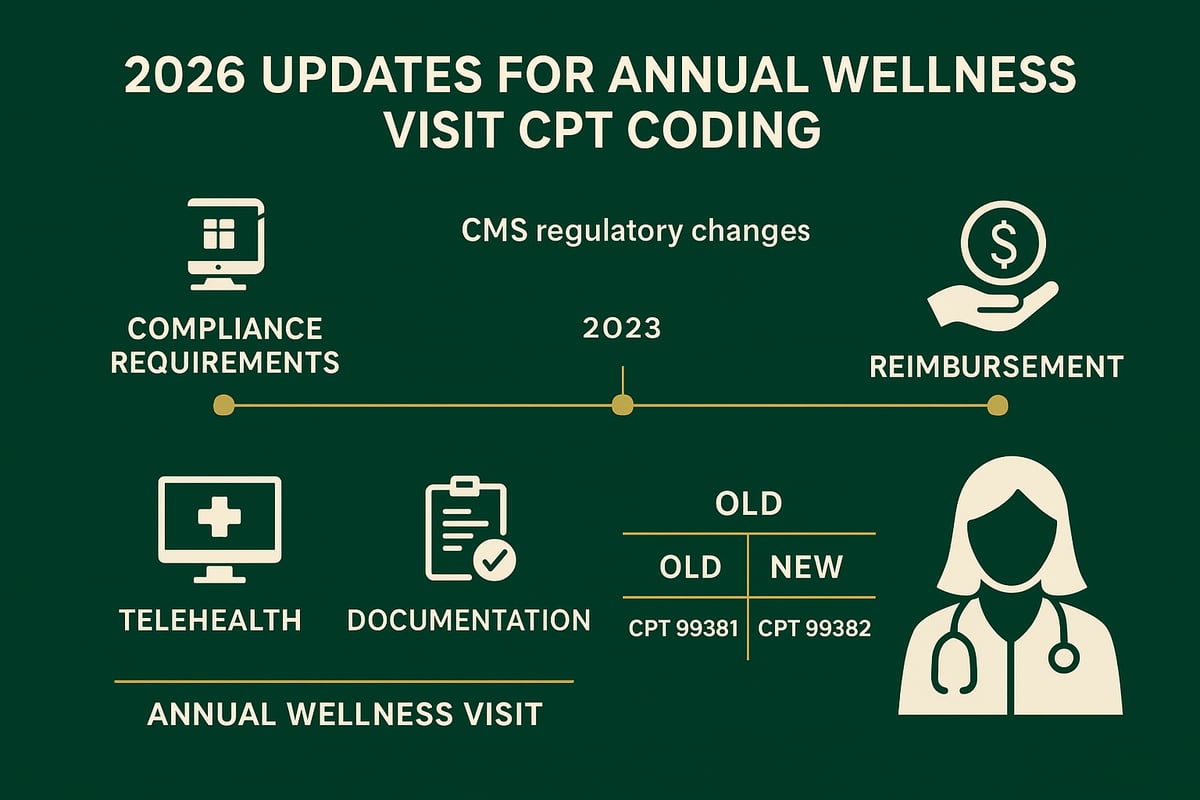
Major Changes to CPT Codes and Documentation in 2026
CMS is expected to introduce significant modifications to the annual wellness visit cpt code by age framework. These include new CPT codes for expanded preventive services, updated definitions for existing AWV codes, and enhanced documentation standards. Practices should review the 2026 CPT Code Updates to ensure they are capturing all billable elements and meeting compliance requirements.
A summary of anticipated 2026 updates:
| Update Area | 2025 Standard | 2026 Expected Change |
|---|---|---|
| CPT Code Set | G0402, G0438, G0439 | New codes for risk-based AWVs, revised descriptors |
| Documentation | HRA, PFSH, screening | Additional risk adjustment, social determinants, digital health documentation |
| Quality Measures | Limited reporting | Expanded quality and outcome reporting requirements |
| Telehealth | Limited flexibility | Broader permanent telehealth options for AWVs |
As the annual wellness visit cpt code by age options expand, documentation will require more detail on patient risk factors, preventive screenings, and digital encounter components.
Telehealth, Reimbursement, and Industry Trends
Telehealth continues to influence AWV delivery. Permanent flexibilities allow AWVs to be conducted via audio-visual platforms, provided all required elements are met. The annual wellness visit cpt code by age must reflect the mode of service, with proper modifiers for telehealth claims.
Reimbursement rates for AWVs may be adjusted based on the 2026 Physician Fee Schedule. Practices should monitor CMS fee schedule updates to anticipate changes in payment. Additionally, value-based care models are increasingly tying AWV performance to quality incentives, making coding precision more important than ever.
Current trends highlight:
- Increased AWV utilization among Medicare beneficiaries
- Higher scrutiny of claim accuracy and supporting documentation
- Expanded use of digital health tools for risk assessment and care planning
Strategic Considerations for 2026 and Beyond
With evolving requirements, organizations must update workflows to align with the annual wellness visit cpt code by age changes. Staff training, template updates, and ongoing compliance reviews are essential. Leveraging expert RCM support can streamline adaptation to regulatory shifts and reduce audit risks.
Staying informed of industry benchmarks and competitor adaptation to AWV CPT code changes will help your organization remain competitive and compliant. By proactively addressing these updates, healthcare providers can maximize AWV reimbursement while ensuring quality patient care.
Best Practices for Accurate AWV Coding and Billing
Accurate coding and billing for the annual wellness visit cpt code by age is essential for healthcare organizations seeking to maximize compliance and reimbursement in 2026. Even minor errors can lead to claim denials, delayed payments, or audit risk. By establishing robust workflows and leveraging proven strategies, your team can streamline AWV billing while reducing costly mistakes.
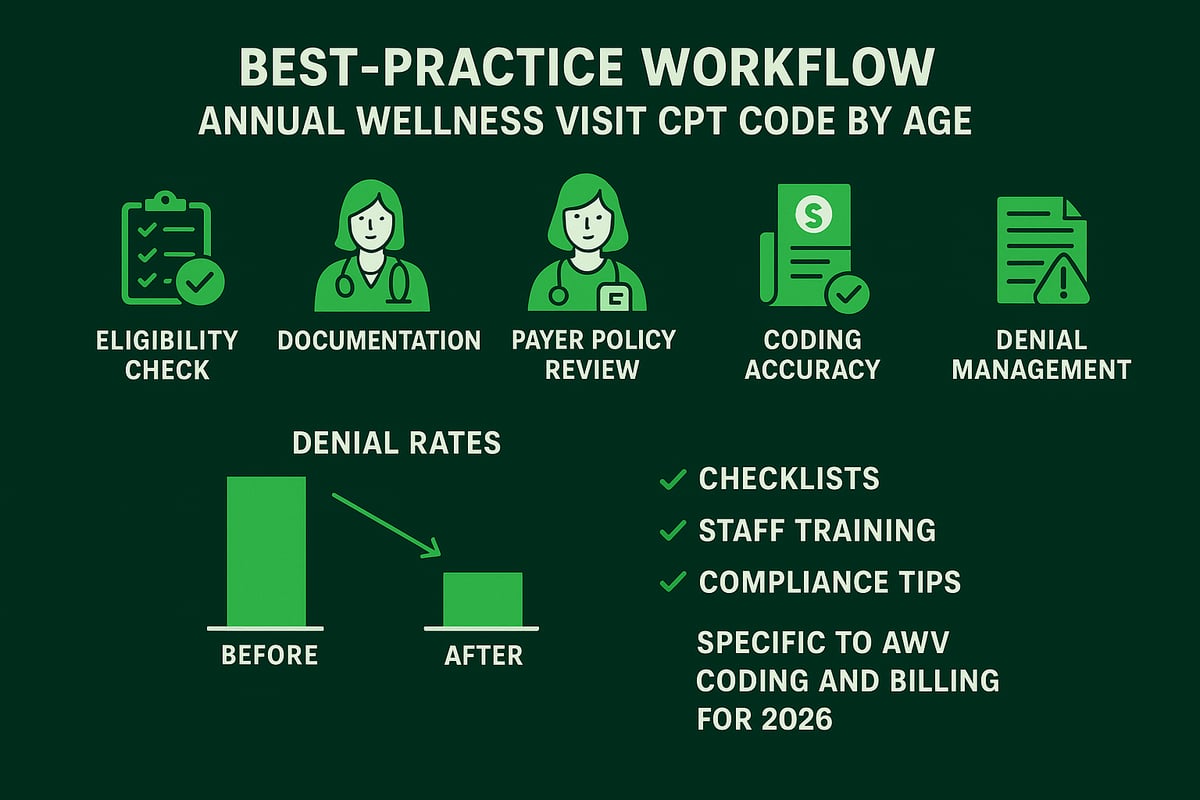
Step-by-Step Workflow for AWV Coding and Billing
Implementing a structured workflow ensures every annual wellness visit cpt code by age is billed correctly. Start with eligibility verification, confirming the patient’s AWV status and payer requirements. Next, collect all necessary documentation, including the health risk assessment and required screenings.
Assign the appropriate CPT code based on the patient’s age and AWV history. For example, use G0402 for IPPE, G0438 for the initial AWV after IPPE, and G0439 for subsequent AWVs. Double-check that any additional preventive services are coded separately but compliantly.
Staff Training and Ongoing Education
Well-trained staff are the foundation of accurate annual wellness visit cpt code by age billing. Regular education sessions help team members stay updated on 2026 CPT changes, documentation standards, and payer-specific nuances. Develop clear protocols for when to escalate coding questions or seek expert guidance.
Leveraging Checklists and Templates
Checklists and documentation templates minimize errors and omissions. Provide your team with standardized forms tailored to each annual wellness visit cpt code by age. These should include prompts for all required elements, such as the personalized prevention plan, screenings, and counseling.
Verifying Payer-Specific Policies
Before submitting claims, verify each payer’s unique policies for the annual wellness visit cpt code by age. Medicare, Medicaid, and commercial insurers may have different eligibility criteria, frequency limits, or documentation expectations. Maintain a payer matrix or quick-reference guide to avoid common pitfalls.
Integrating AWV Coding with EHR and Practice Management
Seamless integration with your EHR and practice management systems can automate parts of the coding process. Ensure your RCM team is adept at using client-owned software to flag missing documentation and prompt for the correct annual wellness visit cpt code by age. This reduces manual errors and speeds up billing cycles.
Real-World Results: Reducing Denials and Boosting Revenue
Practices that follow best practices for annual wellness visit cpt code by age often see up to 15% higher reimbursement rates, according to industry benchmarks. For example, a multi-specialty clinic that implemented checklists and regular training reduced AWV denials by 30% within six months.
The Role of Denial Management and Appeals
Effective denial management is critical for optimizing AWV reimbursement. Proactively tracking denied claims, identifying root causes, and appealing eligible rejections can recover significant revenue. For more on this process, see Denial management in medical billing for strategies to improve cash flow and reduce rejections.
Essential Documentation Checklist
Use this checklist to support every annual wellness visit cpt code by age:
- Patient eligibility and AWV history
- Completed health risk assessment (HRA)
- Required screenings (cognitive, depression, etc.)
- Personalized prevention plan
- Counseling and education provided
- Time and components documented
- Payer-specific forms or attestations
By following these best practices, healthcare organizations can improve compliance, reduce denials, and ensure accurate billing for every annual wellness visit cpt code by age.
Documentation Requirements and Compliance Tips for AWVs
Accurate and thorough documentation is essential for successful billing and compliance with the annual wellness visit cpt code by age. In 2026, evolving payer requirements and increased audit scrutiny make precise documentation more critical than ever. Understanding what to document, where to focus, and how to avoid errors ensures both compliance and optimal reimbursement.
Essential Documentation Components and Best Practices
Each annual wellness visit cpt code by age has specific documentation requirements that must be met to support billing and withstand audits. Key components include:
- Health Risk Assessment (HRA): Collect patient’s medical and family history, lifestyle, and risk factors.
- Screenings and Measurements: Document vital signs, BMI, cognitive and depression screenings, and other age-appropriate assessments.
- Personalized Prevention Plan: Develop and record a tailored plan for disease prevention and health maintenance, including referrals and follow-up needs.
- Counseling and Education: Capture all discussions on risk factors, lifestyle modifications, and community resources.
Documentation must clearly indicate the patient’s eligibility for the specific annual wellness visit cpt code by age, reflecting visit history and payer requirements. Refer to the Medicare Annual Wellness Visit Guidelines for the most up-to-date list of required elements and official definitions.
Common Pitfalls, Compliance, and Audit Trends
Incomplete or inconsistent documentation is a leading cause of claim denials for the annual wellness visit cpt code by age. Omitting required components, such as the HRA or cognitive assessment, can trigger payer audits or recoupments. Failing to differentiate between the Initial Preventive Physical Examination (IPPE) and subsequent AWVs is another frequent error.
Be aware of audit trends highlighted in recent OIG and CMS reports. Auditors often flag visits lacking clear documentation of time spent, eligibility, or preventive plan development. Practices should review the AWV Coding Errors and Compliance resource to understand common pitfalls and industry findings.
Ongoing Monitoring, Templates, and Staff Education
To maintain compliance with the annual wellness visit cpt code by age, implement standardized documentation templates tailored to each age group and visit type. These templates should prompt for all required elements, including screenings, counseling, and the prevention plan.
Regularly audit sample visit notes for completeness and accuracy. Incorporate HIPAA and privacy safeguards in all documentation workflows. Invest in ongoing staff education on regulatory updates, payer-specific requirements, and best practices for supporting the annual wellness visit cpt code by age. Continuous improvement and proactive monitoring are vital for reducing denials and ensuring audit readiness.
Frequently Asked Questions: AWV CPT Codes by Age
Navigating the annual wellness visit cpt code by age is essential for maximizing compliance and reimbursement in 2026. Below, we address the most common questions billing teams and healthcare organizations face regarding AWV CPT coding by age group.
What are the main CPT codes for AWVs in 2026?
The three primary codes are:
- G0402: Initial Preventive Physical Examination (IPPE), for new Medicare beneficiaries within the first 12 months.
- G0438: Initial Annual Wellness Visit, available once after the IPPE.
- G0439: Subsequent Annual Wellness Visits, billed annually after G0438.
| Visit Type | Patient Age | CPT Code |
|---|---|---|
| IPPE (Welcome to Medicare) | New, within 12 months | G0402 |
| Initial AWV | After IPPE, any age | G0438 |
| Subsequent AWV | Ongoing, any age | G0439 |
The annual wellness visit cpt code by age depends on both the patient's age and their visit history with Medicare.
How do I determine which AWV code to use based on patient age and visit history?
Review the patient's Medicare enrollment date and previous AWV claims. Use G0402 for those in their first year, G0438 for the first AWV after IPPE, and G0439 for all following annual visits. For commercial plans, verify policy details as some align with the Medicare structure, but others may vary. Always confirm eligibility before selecting the annual wellness visit cpt code by age.
Can AWV codes be billed with other preventive services on the same day?
Yes, AWV codes may be reported alongside certain preventive services, like depression screening or cognitive assessment, when requirements are met. Ensure all services are documented separately and meet payer criteria. Modifier usage may be necessary to avoid claim edits. For guidance on avoiding common coding mistakes, see Common coding errors in billing.
What documentation is required to support AWV CPT codes?
Documentation must include the health risk assessment, required screenings, counseling, and a personalized prevention plan. Requirements differ by age and payer, so review payer-specific guidelines. Missing or incomplete documentation is a leading cause of denials when billing the annual wellness visit cpt code by age.
How do commercial payers differ from Medicare in AWV coding by age?
While many commercial payers follow Medicare's CPT structure, some have unique requirements or age-based policies for wellness visits. Pediatric and adolescent wellness exams use different CPT codes, and payers may require adherence to guidelines like Bright Futures for patients under 21.
What are the most common reasons for AWV claim denials?
Denials often result from incorrect code selection, missing documentation, or failure to meet eligibility criteria. Regular audits and staff training are essential for reducing errors. For more on how coding impacts reimbursement, explore Revenue cycle management in medical coding.
Are there new changes to AWV CPT codes or requirements in 2026?
Yes, CMS has announced updated documentation requirements, risk adjustment considerations, and modifications to telehealth billing for AWVs in 2026. Stay informed through official CMS publications and industry updates.
Where can I find resources for ongoing AWV coding updates and education?
Visit CMS, payer portals, and industry resources for the latest on annual wellness visit cpt code by age. Partnering with an experienced revenue cycle management team ensures compliance and optimizes reimbursement as guidelines evolve.
If you want to feel confident about your Annual Wellness Visit coding for 2026 and avoid the common pitfalls that lead to denials or lost revenue, you’re not alone. Navigating evolving CPT codes and payer requirements can be overwhelming, but you don’t have to tackle it solo. At Greenhive Billing Solutions, we’re dedicated to helping healthcare providers like you optimize compliance, documentation, and reimbursement—so you can focus on patient care.
Ready to streamline your workflow and boost your practice’s financial health? Book Your Free Consultation and let’s take the next step together.