Healthcare Accounts Receivable Management Services
30% More Revenue with Smart
AR Management
Key Features of Our AR Management Services
Full AR Lifecycle Management
Specialty-Focused Workflows
Real Time AR Monitoring

Your Billing Partner in Revenue Success
Why Providers Trust Greenhive Billing Solutions
From Tempe, Arizona to healthcare practices nationwide, Greenhive Billing Solution is known for recovering AR quickly and transparently. We pair hands on expertise with automation and personal service to improve your collections.
- 30% average boost in revenue recovery
- AR teams trained in Medicare, Medicaid, and commercial payers
- Real time claim tracking and performance updates
- Specialty-specific workflows for better accuracy
- 100% HIPAA compliant systems and secure access
Your AR, Managed Smarter
Our Proven AR Management Workflow
- Secure access to your billing platform
- AR aging report analysis and segmentation
- Prioritized claim follow-up
- Denial Management and Appeals
- Communication with payers and patients
- Reporting, dashboards, and improvement insights
SERVICES
Unpaid Claims Are Quietly Slowing You Down
When reimbursements get stuck, your healthcare practice suffers. Long AR cycles drain revenue, stress your team, and make financial planning difficult. Most providers don’t realize how much income is tied up in unresolved claims and aging balances. That’s where Greenhive’s Medical Billing Services step in. We work behind the scenes, reduce write offs, and get you the payments you’ve already earned.
Stop Losing Revenue to Delays
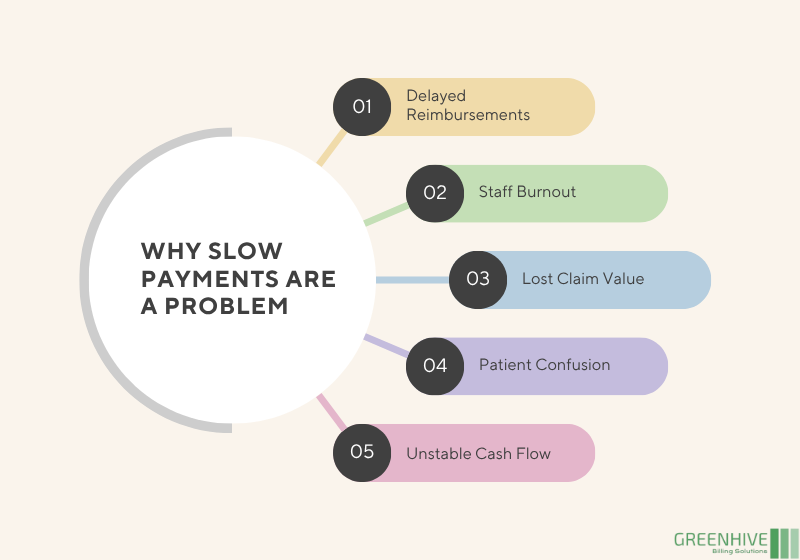
The Real Cost of Aging AR
Why Delayed Payments Hurt More Than You Think Every day a claim goes unpaid, your revenue takes a hit.
Slow AR cycles cause:
- Delayed reimbursements and cash flow problems
- Time-consuming follow-ups by staff
- Missed or underpaid claims slipping through
- Patient frustration over unclear bills
- Unpredictable Claim Revenue planning
Streamline Your Revenue Cycle
What Is AR Management and Why It Matters
Accounts receivable management is more than claim follow-up. It’s a full-cycle process that ensures your hard earned revenue doesn’t get lost in the system. We combine deep billing knowledge with real time tracking to resolve aging balances and prevent delays.
Our AR specialists manage the entire revenue chain:
- AR aging analysis and prioritization
- Insurance and patient follow-ups
- Denial handling and appeals
- Insurance verification and eligibility checks
- Payment Posting and reconciliation
- Actionable reports and performance insights
Whether you’re a small clinic or a large group practice, outsourcing accounts receivable management helps reduce internal workload, increase recoveries, and streamline your revenue cycle.
BENEFITS
Benefits of Our AR Management Services
Higher Collection Rates
We pursue every dollar, no claim is left behind.
Faster Reimbursements
Reduce your AR days with streamlined, proactive follow-up.
Fewer Denials
We resolve rejections and prevent future ones with workflow improvements.
Stronger Cash Flow
Consistent collections mean fewer financial disruptions.
Aging AR Hurts More Than You Know
When claims sit unpaid for 60, 90, or even 120 days, the chances of recovery drop fast. That’s why it’s crucial to stay ahead, tracking every claim, resolving issues quickly, and working closely with your team to prevent revenue loss before it starts.
Updated July 2025: AR Management Trends
Lately, we’ve noticed a clear shift in what providers expect from AR. It’s no longer just about following up on old claims. It’s about staying ahead. Real-time tracking, smarter dashboards, and closer connections between billing, coding, and eligibility are becoming the standard. More teams want insights they can act on immediately, not just reports that arrive after the damage is already done. As value-based care continues to grow, efficient AR is no longer just about finances. It’s becoming a key part of delivering better patient care.
We Work With Payers, So You Don’t Have To
Each payer has its own rules. Medicare, Medicaid, Blue Cross, Aetna, we handle them all. Our team stays on top of industry changes and payer updates, so your claims move faster with fewer delays.
We manage:
- Aged claim recovery (30–120+ days)
- Denied or underpaid claims
- Eligibility and coverage problems
- Missing documentation follow-up
- Timely resubmissions and appeal deadlines
OUTCOMES
Results That Speak for Themselves

Let’s Turn Denials into Dollars
Let’s Recover What You’ve Already Earned
ANY QUESTIONS?
Frequently Asked Questions
What’s the difference between AR management and billing?
Can AR services recover old claims?
Do you support specialty practices?
How fast can you recover aging AR?
How do you stay updated with payer rules?
Why outsource AR instead of doing it in-house?