Healthcare Revenue Reporting & Analytics
See Denials Before
They Happen
How Our Healthcare Revenue Cycle Management Analytics Deliver Results
End-to-End Eligibility Oversight
From insurance lookup to real-time claim outcomes, we cover it all.
Customized Analytics by Specialty
Live Eligibility Dashboards

Turn Analytics into Action
Why Providers Trust Greenhive Billing Solutions
- 25–40% drop in eligibility related denials
- Seamless EHR and billing platform integrations
- Specialty-specific data filters and benchmarks
- Alerts for trends and recurring payer issues
- 100% HIPAA-compliant reporting systems
Your data holds the answers, Greenhive helps you read them.
From Data to Actionable Insights
Our Proven Revenue Cycle Analytics Workflow
- Secure access and setup
- Eligibility data extraction
- Payer performance analysis
- Issue tracking and alerting
- Dashboard creation and team training
- Ongoing updates and optimization
SERVICES
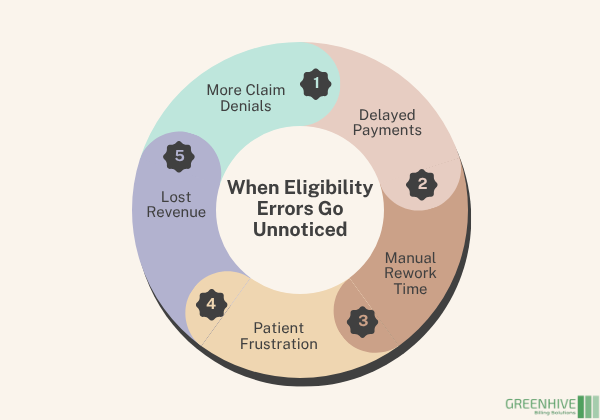
Hidden Errors Are Hurting Your Revenue
When eligibility issues go unchecked, claims get denied and payments get delayed. The problem? Most practices don’t realize where verification breaks down until it’s too late. Without proper visibility, bad data flows through your entire billing cycle.
That’s where Greenhive Billing Solutions comes in. We use real-time reporting and analytics to uncover risks, spot trends, and fix eligibility issues before they impact your bottom line.
Accuracy Protects Revenue
Why Missed Eligibility Checks Cost You
- Increased claim denials and rework
- Payment delays due to missing info
- Hours wasted on manual verification
- Frustrated patients and surprise bills
- Missed revenue opportunities
Eligibility Reporting That Matters
What Is Eligibility Reporting, and Why It Matters
Eligibility analytics go far beyond yes/no insurance checks. We deliver meaningful insights that help you optimize verification, reduce denials, and increase first-pass claim success.
With Greenhive, you get data-driven precision at every step:
- Real-time eligibility failure tracking
- Insurance verification performance reporting
- Denial trend identification
- Payer specific compliance insights
- Patient coverage validation metrics
- Easy to understand dashboards
With our tools and support, your team doesn’t just verify, they strategize.
BENEFITS
Benefits of Our Revenue Cycle Management Analytics
Fewer Claim Denials
Spot errors and trends before they trigger rejections.
Faster Claim Approvals
Submit clean claims the first time with verified data.
Better Patient Experience
Fewer billing surprises mean happier patients.
Reduced Admin Burden
Automated tracking saves time and improves accuracy.
Inaccurate Eligibility = Delayed Revenue
When eligibility issues aren’t tracked, they repeat. Claims get denied, resubmissions get delayed, and your team stays stuck in reactive mode. Greenhive changes that with a proactive, data first approach that eliminates blind spots and boosts cash flow.
Stay Ahead of Payer Changes
Medicare, Medicaid, commercial payers, each one changes fast. We stay on top of evolving rules, update your workflows, and notify your team before problems happen.
We manage:
- Eligibility denial trend reporting
- Insurance verification success metrics
- Missed/mismatched coverage detection
- Recurring payer error patterns
- Real time alerts for denied eligibility
OUTCOMES
Results That Speak for Themselves

Let’s Eliminate Preventable Denials
Make Eligibility Your Revenue Advantage
Denial prevention through analytics ensures bad insurance data doesn’t cost you revenue. Our team makes sure you never miss what matters.
ANY QUESTIONS?
Frequently Asked Questions
What is reporting and analytics in eligibility verification?
How does analytics improve claim accuracy?
Do you support small practices or solo providers?
Is this integrated with my billing platform?
How secure is the data?