Medical Insurance Claims Processing Services
Protect Your Cash Flow with
Clean, Timely Claims
Complete Medical Insurance Claims Processing for Healthcare Providers
Medical insurance claims processing is one of the most critical steps in the healthcare revenue cycle. When claims are delayed or denied, it directly impacts your cash flow. At Greenhive Billing Solutions, we help healthcare providers across the United States streamline claims submission and ensure faster reimbursements with specialty-specific workflows.
End-to-End Claims Management
Specialty-Aware Submissions
We tailor submissions to the medical coding needs of your field whether it’s orthopedics, cardiology, or primary care.
Active Reimbursement Follow-Up
We don’t just submit, we track payments, post accurately, and escalate delays.

Claims Processed Right, Every Time
Why Healthcare Providers Choose Our Medical Claims Processing Services
- 99% Clean Claim Rate
- Certified Claims Specialists & Billers
- Full HIPAA-Compliance
- Daily Rejection Monitoring & Appeals
- Custom Workflows for Your EHR & Specialty
- Transparent Submission & Payment Reports
Efficient Claim Submission
Our Proven Claim Submission Workflow
- Patient & Policy Verification
- Procedure & Diagnosis Code Review
- ANSI 837 Formatting & Validation
- Electronic Submission to Payers
- Real Time Reimbursement Monitoring
- Payment Posting & Denial Follow-Up
SERVICES
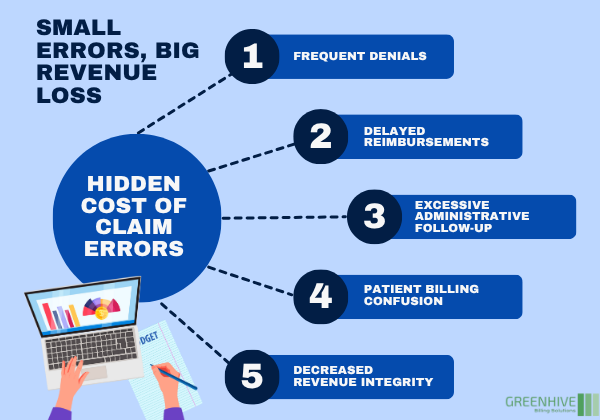
Billing Delays Are Quietly Draining Your Revenue
Unpaid claims. Rejected submissions. Endless follow-ups. Sound familiar?
Disorganized billing processes cause thousands in lost revenue and wasted staff hours. Even one missing detail in a claim can hold up payment for weeks. That’s why providers across the country choose Greenhive Billing Solutions to handle claim submission and reimbursement with precision, so payments don’t slip through the cracks.
Protect Your Revenue, Simplify Billing
Why Submission Errors Cost More Than You Think
- Frequent denials and rejections
- Delayed reimbursements
- Excessive administrative follow-up
- Patient billing confusion
- Decreased revenue integrity
Accuracy Drives Revenue
Understanding Medical Claims Submission and Reimbursement
It’s not just paperwork. It’s your payment pipeline.
Claim submission and reimbursement involve documenting services, coding them accurately, submitting to payers, and ensuring timely payment. Any mistake, whether in formatting, coding, or communication, can trigger a denial.
Our specialists are trained in payer-specific rules, ANSI 837 formats, and specialty workflows. We ensure your claims are accurate, complete, and ready for fast approval.
BENEFITS
Benefits of Submission & Reimbursement Services
Higher Approval Rate
We get it right the first time, reducing rejections and resubmissions.
Faster Reimbursements
Quick, clean electronic submissions mean faster payment turnaround.
Reduced Denials
Denial Management Service ensures that every claim is reviewed for accuracy before submission.
Less Staff Burden
We catch missed charges and reduce unbilled services.
Turn Your Claims Process Into a Revenue Engine
We Handle the Complexity, So You Don’t Have To
OUTCOMES
Results That Matter

Clean claims. Faster payments. Less stress.
Let’s Fix the Leaks in Your Revenue Cycle
ANY QUESTIONS?
Frequently Asked Questions
What is claim submission and reimbursement in healthcare?
Why are clean claims so important?
Can you integrate with our EHR?
Do you handle appeals and resubmissions?
Is your service HIPAA-compliant?
What are the benefits of outsourcing health insurance claims processing?
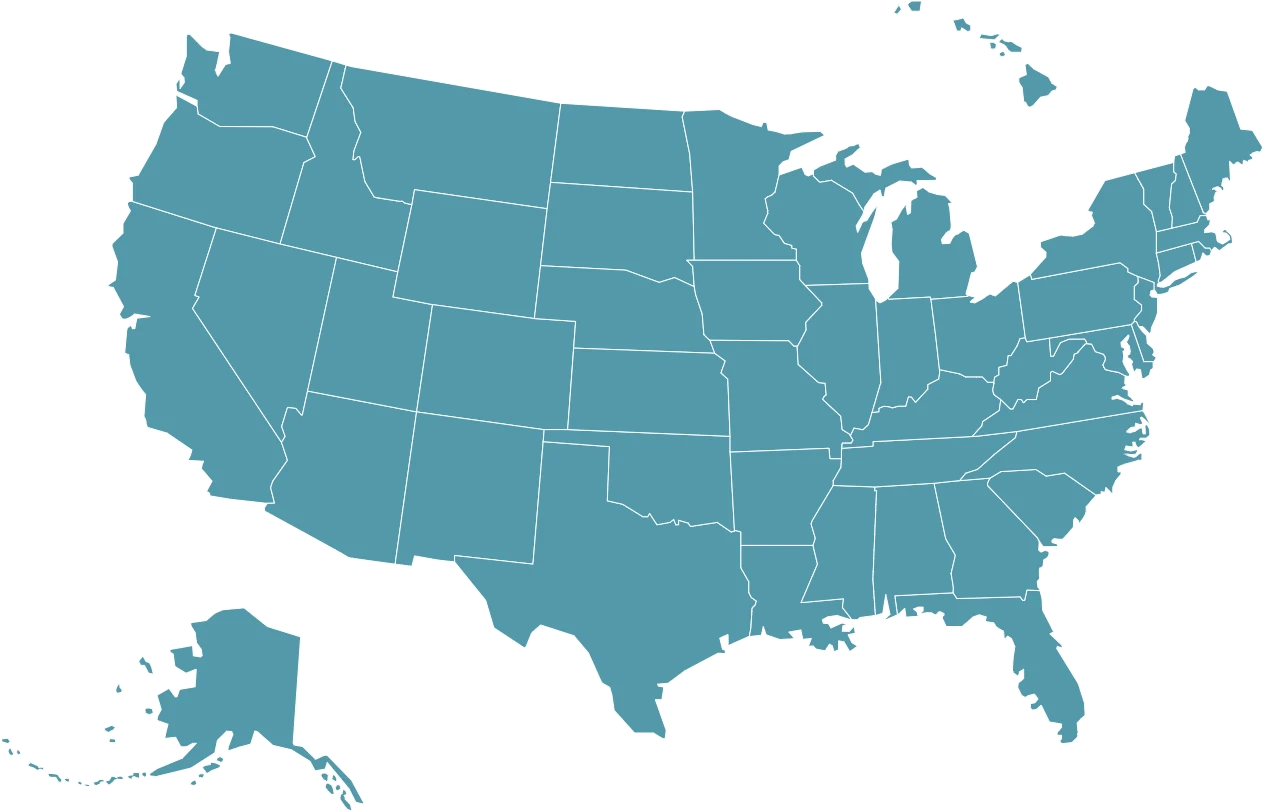
WE SUPPORT
Trusted by Providers Nationwide
Greenhive Billing Solutions supports healthcare practices in every state from our Arizona location. Whether you’re a solo provider or a multi-location chain of hospitals or clinics, we deliver scalable claim support that keeps your revenue strong.
